Introduction
Despite improvements in survival and life expectancy in high-income countries, adolescent and young adults (AYAs) living with sickle cell disease (SCD) remain at significant risk for morbidity and mortality. Our previous work using group-based trajectory modeling (GTBM) has demonstrated that a subset of AYAs with SCD are at risk for significant morbidity with SCD with increased healthcare utilization, vasoocclusive pain episodes, and death, particularly after transition to adult care (Kayle et al., Pediatric Blood & Cancer, 2018). Yet, there is limited insight into which AYAs with SCD are at high risk for poor outcomes. The objective of this study was to identify patterns of emergency department (ED) utilization of AYAs with SCD in NC as individuals age, with the overarching future goal of better predicting which individuals are at highest risk.
Methods
The NC Hospital Discharge Data (Inpatient, Ambulatory Surgery/Outpatient and ED Databases), 2013-2020 were used. A patient with SCD was defined as a patient who had three or more visits (inpatient, ambulatory surgery, or ED visit) with International Classification of Diseases 9 or 10 codes for SCD within a 5-year period. Date of birth, sex and zip code were used to link patients across the datasets. Demographic variables including age, sex, race and ethnicity were extracted from visit level data. ED visits were defined as all ambulatory ED visits and ED visits that resulted in inpatient admissions between 2013 and 2019. Descriptive statistics were calculated to describe the sample characteristics such as sex and race. The number of ED visits per year across age 14 to 30 years were used as longitudinal variables in GTBM to identify trajectories of latent classes of ED visits. The number of latent classes was determined by model-fit indices such as BIC and entropy.
Results
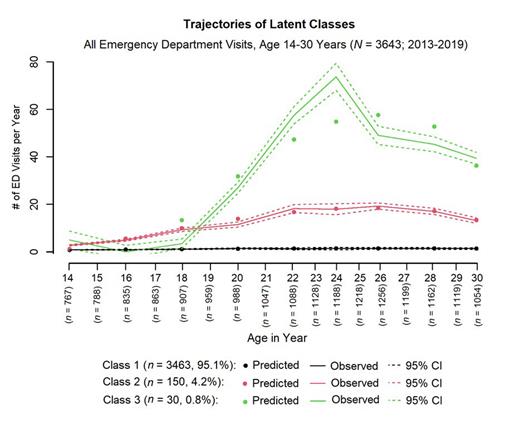
There were 3643 participants included in this study. Participants were 95% Black or African American, 53.8% female and 46.2% male, with age ranging from 14-30 years. Our GTBM models identified three latent classes of participants (Figure 1) with similar ED utilization at age 14 years, but divergent predicted annual ED trajectories beginning around 18 years of age. Class 1, comprising 95% of the participants (n=3463) and 54% female, had minimal ED utilization throughout all the years. Class 2, comprising 4% of the participants (n=150) and 51.3% female, had a steady increase in annual ED use, peaking at 20 visits per year by at age 24 years. Class 3, comprising 0.8% of the participants (n=30) and 47% female, had more extreme ED utilization, up to 80 visits per year at age 24 years.
Conclusions
Using a large longitudinal dataset, we demonstrate distinct patterns of ED utilization among AYAs with SCD by age. Although ED utilization was similar between the groups at age 14 years, a small proportion (~5%) of individuals accounted for the highest ED utilization at older ages. Additionally, amongst the patients with highest ED utilization, there was a marked increase in ED utilization from age 18-24 years, highlighting the highest risk ages within the AYA population, when there is often a transition from pediatric to adult care. There were slightly more males in the highest ED utilization class, highlighting potential gender differences in ED utilization. Our next steps will be to assess which clinical and social factors predict ED utilization trajectory. Limitations in this study include the use of hospital discharge datasets, which may have limited the capture of patients with infrequent acute care visits and limited our ability to examine the role of SCD genotypes and disease-modifying therapy use on ED utilization patterns. Despite these limitations, the study identifies distinct classes of ED use among AYAs with SCD. Understanding and predicting patterns of ED utilization are critical in targeting early interventions towards individuals with the highest risk of healthcare utilization and disproportionate risk for future morbidity.
Disclosures
Desai:University of Tennessee: Research Funding; University of Pittsburgh: Research Funding; PCORI: Research Funding; NIH: Research Funding; Novartis: Research Funding, Speakers Bureau; POC Detection of Hemoglobin Sickling via Magnetic Fractionation: Patents & Royalties: (Pending); US Food & Drug Administration: Research Funding; Chiesi: Consultancy; Vertex: Consultancy; Forma Therapeutics: Consultancy.